Kids Health Update 2025
What local experts say
Kids and Heat
Avoiding heat stroke, heat exhaustion and the irritation of sunburn
Pia B. Fenimore, MD
Lancaster Pediatrics

As we endure the hot summer months — especially as children begin practicing school sports and participating in marching band — it’s important to take steps to avoid heat exhaustion and heat stroke.
Heat stroke is defined as a core body temperature higher than 104°–105°, combined with central nervous system symptoms such as confusion, fainting or severe headache. Heat exhaustion is the precursor to heat stroke and includes symptoms such as profuse sweating, nausea, vomiting, headache, weakness, dizziness, increased thirst and decreased urine output.
It’s important to note that children — especially infants and athletes — are more susceptible to heat illness than adults. And August is by far the most common month for heat-related illness, with two-thirds of all emergency department visits for this condition occurring then. Add to that the rising incidence of heat stroke in the United States, with about 125,000 emergency visits reported in 2023.
Some Things to Know
The heat index is a measure of both temperature and humidity and classifies environments into various danger zones. Find the heat index on the National Weather Service website, Weather.gov/Safety/Heat-Tools.
Hydration is critical during heat exposure. Here are some guidelines for sports: children 9 to 12 should drink 4 to 8 ounces every 20 minutes, and adolescents should drink 40 to 50 ounces per hour. Alternating between water and electrolyte drinks, such as Gatorade, is a good strategy to maintain electrolyte balance without adding too much sugar.
Acclimatizing to heat is possible over a few days to weeks. This means children and teens can gradually increase the intensity or duration of their activities in the heat. Older children can usually acclimatize in four to five days, but younger children may take longer, 10 to 14 days.
Prescription medications require extra caution, for example if a child takes medication for attention deficit disorder or uses creatinine supplements.
Sports equipment, such as pads and other gear that increase heat retention, also put young athletes at an increased risk of heat illness.
Heat Illness Is Preventable
Parents and coaches should take steps to ensure children are safe from the heat:
- Get to know the heat index and restrict activities on days labeled Danger.
- Take frequent hydration breaks, according the kids’ ages and needs.
- Do frequent player substitutions during games to allow for rest.
- Have shaded rest areas.
- Change practice times to earlier or later in the day, with cooler temperatures and less humidity.
- Allow for a complete rest and cooldown after activity.
- Don’t allow children to play if they’re ill, including gastrointestinal symptoms such as diarrhea.
Prompt recognition of heat exhaustion is critical to avoid it becoming heat stroke. If a child is showing signs of heat illness, stop exercising, move the child to a cooler environment immediately and give the child chilled, salt-containing liquids (such as Gatorade). If symptoms aren’t responding, seek advanced care.
Special Handling for Babies
Because babies don’t have the ability to cool their body well and have a higher surface area, they are more susceptible to heat illness and progress faster to heat stroke than older children. Complicating matters, babies may not always show obvious signs of heat exhaustion and instead show subtle symptoms such as fussiness, decreased feeding, fewer wet diapers or lethargy.
When the heat index is about 75°, take these steps to prevent serious heat-related complications in infants:
- Avoid sun exposure and stay indoors during peak heat.
- Dress them appropriately for the heat (loose, light-weight, light-colored clothing).
- Breastfeed or bottle-feed babies more frequently (don’t give water without consulting a pediatrician).
- Cool them down with damp cloths and fans (but not blowing directly on them).
- Never leave a baby in a parked car, even with the windows open.
Sunburn
Sunburns are another summer concern. In addition to the immediate discomfort, repeated sunburns can put your child at increased risk for skin cancer. Although one sunburn doesn’t cause skin cancer, repeated burns do. And since melanoma is the second most common form of cancer in young adults ages 15 to 20, take precautions.
Always apply sunscreen with at least SPF 30, and reapply every two hours and after swimming.
How does sunburn happen? Photo damage from the sun to the skin cells’ DNA triggers an immune response, which creates the body’s response to the burn. Symptoms can begin anywhere from 30 minutes to 24 hours after sun exposure, with redness peaking at 12 to 24 hours, and typically gone in 72 hours.
Other common sunburn symptoms include pain, swelling, blistering and increased sensitivity to heat. Blistering indicates the burn reached the deeper layers of skin. Note that certain medications, such as antibiotics, can increase sun sensitivity and may result in more severe sunburns.
Sunburn Relief
Generally, sunburns resolve naturally over three to four days, so treatment is aimed at controlling symptoms, particularly pain. Cool compresses can help alleviate the sting. Blisters should be allowed to rupture on their own, and once they do, the area should be gently cleaned with soap and water. Then watch for signs of infection.
Since sunburn is an inflammatory reaction, NSAIDs (ibuprofen) are helpful in relieving discomfort, though topical steroids (cortisone) don’t appear to reduce pain or swelling. Aloe vera-based gels are effective for cooling the skin, but avoid products that contain lidocaine, which cause unwanted side effects. Calamine lotion, a soothing topical treatment made from a zinc mixture, is both safe and effective.
Home remedies for sunburn mostly aim at increasing the pH of the skin to promote better healing and reduce irritation. Baking soda, raw potatoes and oatmeal are natural options that may help soothe sunburned skin.
After a day or two, many sunburns will begin to peel, as the body sheds skin damaged by the burn. Moisturizing can slow, but not prevent, the peeling. Keeping the skin moisturized also helps reduce the itching.
Since sunburn can affect our ability to cool ourselves, it’s important to keep children indoors and avoid further heat exposure until symptoms have resolved. Staying hydrated helps maintain adequate blood flow to the skin to promote healing.
As a pediatrician, I always want kids to go outside and be active, as studies show time outdoors helps prevent joint problems, obesity, diabetes, anxiety and depression. But the heat index and risk of heat illness mean adults need to think about preparing children for heat exposure before sending them outside. With just a few adjustments, plenty of hydration and a prevention mindset, it’s still possible for kids to safely participate in outdoor activities — even during hottest summer months!
 Pia B. Fenimore, MD, is a general pediatrician at Lancaster Pediatrics and the vice chair of pediatrics at Penn Medicine Lancaster General Hospital. She has contributed to numerous publications, presentations, committees and community health projects in pediatrics and is a proud mother of two boys. She received her medical degree from Sidney Kimmel Medical College at Thomas Jefferson University and has been in practice for more than 20 years. PennMedicine.org
Pia B. Fenimore, MD, is a general pediatrician at Lancaster Pediatrics and the vice chair of pediatrics at Penn Medicine Lancaster General Hospital. She has contributed to numerous publications, presentations, committees and community health projects in pediatrics and is a proud mother of two boys. She received her medical degree from Sidney Kimmel Medical College at Thomas Jefferson University and has been in practice for more than 20 years. PennMedicine.org
Summer Means Ticks
The season is getting longer and worse, especially for Lyme disease in our area
Ericka Hayes, MD
Children’s Hospital of Philadelphia
 Warm weather brings the pleasures of increased outdoor activities. But it also brings the pain of increased infections transmitted by ticks and mosquitoes.
Warm weather brings the pleasures of increased outdoor activities. But it also brings the pain of increased infections transmitted by ticks and mosquitoes.
Ticks and mosquitoes, unfortunately, are quite good at spreading diseases that can cause serious illnesses. In spring and summer, ticks are emerging from larvae into their tiny nymph form, which makes it easy for you to pick up ticks without noticing.
Here’s what to know to help prevent an unwanted infection.
Common Local Infections
There are many infections transmitted by ticks and mosquitoes, many of which have distinct geographic distributions, including some seen primarily outside the U.S. But with global warming and the ongoing spread of ticks, mosquitoes and their host animals, we continue to see evolution in the distribution of these infections — including more in our area. It’s also important to recognize the risk of travelers carrying these infections from outside our area.
As you may be aware, Lyme disease is the most common tick-related infection we see in our area as well as in the entire U.S., though it’s limited to certain regions. In 2023 (the most recent data available) there were about 90,000 cases of Lyme nationwide. For Pennsylvania, there were 16,671 reported cases, second only to New York for total cases. New Jersey had 7,224 cases.
Other less commonly seen tick-transmitted infections include anaplasmosis, babesiosis, ehrlichiosis and Powassan. Other parts of the U.S. see Rocky Mountain spotted fever, tularemia, as well as significantly more ehrlichiosis than our region. Rocky Mountain spotted fever, anaplasmosis and ehrlichiosis can all cause life-threatening infections.
Overall, mosquito-related infections are less common than tick infections in the U.S. For mosquitoes, the most common infection we see in all regions is West Nile virus infection. This fortunately tends to be mild in children but can be severe in immunocompromised persons and the elderly. Other less common mosquito-transmitted infections found locally include eastern equine and Jamestown Canyon viruses, which can cause severe neurologic complications.
Internationally, malaria and dengue are the two dominant mosquito-transmitted infections that can be life threatening. Zika, Oropouche and chikungunya are also potentially serious mosquito-borne infections, particularly for pregnant individuals and their infants.
Symptoms of Bug-Related Illnesses
The symptoms of both tick- and mosquito-related illnesses are nonspecific, making it difficult to diagnosis these infections at early stages. Fever is common, along with fatigue, body aches and headaches (particularly for Rocky Mountain spotted fever).
Lyme disease has a characteristic expanding red rash centered on the tick bite site, sometimes with central clearing that appears eight to 14 days after the bite. A rash is also seen in Rocky Mountain spotted fever (the “spotted” part of the name), starting on the extremities with lesions involving the palms and soles.
The incubation period (time from bite until a person gets sick) for most tick- and mosquito-related infections ranges between two days to four weeks, depending on the specific infection.
Prevention
The good news is that most tick and mosquito infections are preventable. For both ticks and mosquitoes, avoiding bites is the best way to avoid getting sick. Tools to do this include using insect repellant such as DEET (note higher concentrations are required to repel ticks compared with mosquitoes), avoiding being outside during peak biting times (dusk, dawn, nighttime), as well as using insect repellent devices if you must be outside.
For outdoor activities, wear closed-toe shoes, socks and tuck pants into socks to minimize ticks attaching to your body. Clothing can be sprayed with permethrin (another insecticide) or purchased already treated with permethrin. Walking in the center of trails to avoid tall grasses, bushes and wooded areas also helps avoid contact with ticks and insects.
At your home, keep your grass cut short. To decrease mosquitoes breeding near your home, dump out any standing water, and keep your gutters clear. After returning from outdoor activities, the first step is to check your clothing for ticks and then wash your clothing in hot water and fully dry it on high heat.
Ticks must be attached and feed on a person for a minimum of 12 to 24 hours to transmit most infections, so removing ticks promptly eliminates the risk of most tick-borne infections. For your protection, shower within two hours of completing outdoor activities to rinse away unattached ticks. In addition, perform a thorough full-body check for attached ticks. Be sure to check areas where ticks often hide, including under arms, in and around ears, in the belly button, back of knees, in and around hair, between legs and at the waist.
Remember to check pets that go outside as well. Young nymph ticks are quite small (about 1 mm), so close inspection is needed.
See more information on tick prevention from the CDC at CDC.gov/Ticks/Prevention.
Tick Removal
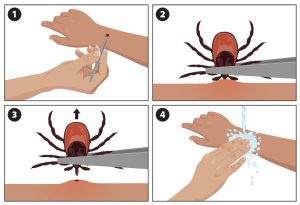
If you find an attached tick, it’s important to remove it as soon as possible (remember the 12- to 24-hour attachment window for most infection transmissions). To remove an attached tick, grasp the tick as close to the skin surface as possible with clean finetipped tweezers. Pull up at a 90° angle, perpendicular to the skin (see image) with steady pressure without twisting. Twisting or jerking can lead to the tick mouth parts breaking off in the skin. If this happens, remove them with tweezers if you can do so easily. If not, they will be pushed out as the skin heals.
Don’t use petroleum jelly, heat, nail polish or other techniques to try to make the tick detach itself. This may agitate the tick and force infected fluid from the tick into the skin.
Dispose of the tick safely by flushing it or putting it in a sealed container. Don’t crush or pop ticks as this is an infection risk. Finally, clean the skin at the bite site with soap and water or alcohol and wash your hands thoroughly
Treatment
If you suspect you or your child may have a tick- or mosquito-related infection, reach out promptly to your primary care provider. Many tick illnesses, such as Lyme disease and Rocky Mountain spotted fever, are treatable with antibiotics.
For international travelers, malaria has specific treatment available. If you suspect you may have malaria, seek care immediately as this can be a life-threatening illness. Unfortunately, some tick- and most mosquito-borne viral infections don’t have specific treatment aside from supportive care.
The wonderful warm weather of this season is for all to enjoy. Don’t let ticks and mosquitoes ruin the fun. Taking proactive steps to avoid bites and doing regular tick checks will help you stay safe.
 Ericka Hayes, MD, is senior medical director of Infection Prevention at Children’s Hospital of Philadelphia (CHOP) and a professor of clinical pediatrics at the University of Pennsylvania Perelman School of Medicine. She’s a graduate of Washington University School of Medicine and has more than 25 years of experience in pediatric infectious diseases, include at the pediatric HIV program at St. Louis Children’s Hospital. CHOP.edu.
Ericka Hayes, MD, is senior medical director of Infection Prevention at Children’s Hospital of Philadelphia (CHOP) and a professor of clinical pediatrics at the University of Pennsylvania Perelman School of Medicine. She’s a graduate of Washington University School of Medicine and has more than 25 years of experience in pediatric infectious diseases, include at the pediatric HIV program at St. Louis Children’s Hospital. CHOP.edu.
A Parent’s Guide to Tongue-Tie
Laura Eisel, PA-C, MMS
Nemours Children’s Health

Tongue-tie is a condition that can affect movement of the tongue. It occurs when the lingual frenulum — the thin band of tissue that connects the underside of the tongue to the floor of the mouth — is too short, too tight or connected to the tip of the tongue. This can limit the tongue’s movement, potentially causing problems for both babies and older children.
As a parent, it’s helpful to be aware of the signs, as well as diagnosis and treatment options associated with tongue-tie.
Overview
Tongue-tie is a congenital condition, meaning it’s present at birth. The lingual frenulum is a normal structure but, in some cases, it can be abnormally short or thick, or it may connect to the very tip of the tongue. This may limit the tongue’s ability to move freely.
This condition can affect feeding, speech and other oral functions. The severity of tongue-tie can vary widely, from mild cases that typically don’t require treatment, to more severe cases that can significantly impact a child’s quality of life.
Problems
In newborns, tongue-tie can cause difficulties with breastfeeding. The restricted tongue movement can make it hard for the baby to latch onto the breast properly or feed effectively. This may cause prolonged feedings, poor milk transfer, nipple pain for the mother and inadequate weight gain for the baby. In some instances, infants may also have trouble bottle-feeding, as they can’t form a proper seal around the bottle’s nipple.
In older children, tongue-tie can affect speech. It doesn’t cause a delay in babbling or speech development but may affect articulation and clarity of speech. The tongue’s limited movement can make it difficult to pronounce certain sounds, such as “l,” “t,” “d” or “n.”
Also, tongue-tie can cause issues with oral hygiene, as the tongue may not be able to effectively clean the teeth and mouth, leading to cavities despite good brushing habits.
Diagnosis
Diagnosing tongue-tie involves a physical examination by a healthcare provider. For newborns, this is often done following birth or during routine checkups. The provider will look at the underside of the baby’s tongue and assess the range of motion.
In older children, a speech-language pathologist or an ear, nose and throat specialist (ENT) may be involved in the diagnosis. The specialists will evaluate the child’s speech and oral function to determine if tongue-tie is the underlying cause of any issues.
Treatment Options
For mild cases of tongue-tie, nonsurgical treatments may be recommended. These can include breastfeeding support from a lactation consultant who can provide techniques and strategies to help the baby feed more effectively. For older children, speech therapy with a speech-language pathologist can help to improve speech and oral function through exercises and special techniques.
For more severe cases, surgical intervention may be necessary. The two main procedures are frenotomy and frenuloplasty. A frenotomy is a simple procedure that involves cutting the lingual frenulum to release the tongue. For newborns, this may be done in an outpatient office and takes only a few minutes to complete.
A frenuloplasty is a more complex procedure performed under general anesthesia. The lingual frenulum is cut and the wound edges are reapproximated using stitches underneath the tongue. Recovery typically takes several days.
If you think your child has tongue-tie, it’s important to see a doctor for a diagnosis. The sooner the condition is diagnosed and treated, the better the chances of successful treatment and prevention of long-term complications. In newborns, look for signs of difficulty latching, poor milk transfer or inadequate weight gain. In older children, watch for signs of impaired speech articulation, difficulties pronouncing certain sounds or oral hygiene issues.
Complications of Untreated Tongue-Tie
If left untreated, tongue-tie can lead to a range of complications. Symptoms that older children or adults may experience include feeding difficulties, oral hygiene issues, and possible social and emotional repercussions.
The age for treatment depends on the severity of the condition and the age of the child. For newborns, a frenotomy is often performed within the first few weeks of life to address feeding issues. In older children, the timing of treatment may be more flexible and can be determined based on the child’s speech and oral function needs. Early intervention is generally recommended to prevent longterm complications.
Follow-Up Care
After treatment, follow-up care is essential to ensure proper healing and to monitor the child’s progress. For newborns, this may involve continued breastfeeding support and regular checkups with the pediatrician. For older children, follow-up care can include speech therapy sessions and regular evaluations by the speech-language pathologist or a pediatric otolaryngology (ear, nose and throat) specialist.
Tongue-tie is a condition that can significantly impact a child’s feeding, speech and overall well-being. If you suspect your child has tongue-tie, don’t hesitate to seek medical attention. With proper diagnosis and treatment, your child can overcome the challenges of tongue-tie and develop healthy feeding and speech patterns. Early intervention and proper treatment can make a significant difference in a child’s quality of life.
Some Controversy
Whether or not to treat tongue-tie can be controversial. The severity of tonguetie and severity of symptoms don’t always align. For example, a child may have a severe degree of tongue-tie and yet not exhibit any feeding or speech difficulties. In this case, observation and no surgical intervention may be pursued. In other cases, the degree of tongue tie may be milder but result in symptoms with significant impact on the quality of life. Here, the procedure is recommended.
Every child is unique, and all factors need to be considered when deciding on a best treatment course with your healthcare provider.
 Laura Eisel, PA-C, MMS, has been a Physician Associate in Pediatric Otolaryngology at Nemours Children’s Health for nine years. She completed her undergraduate education at Penn State University and received her master’s degree from Arcadia University. She’s certified by the NCCPA and is a member of the Society of PAs in ENT. For more, visit Nemours.org.
Laura Eisel, PA-C, MMS, has been a Physician Associate in Pediatric Otolaryngology at Nemours Children’s Health for nine years. She completed her undergraduate education at Penn State University and received her master’s degree from Arcadia University. She’s certified by the NCCPA and is a member of the Society of PAs in ENT. For more, visit Nemours.org.
